"Our cold plasma system basically suppressed the supply lines to cancer cells to result in their death," said Michael Kong, Batten Endowed Chair in Bioelectrics at ODU. "Importantly, the cold plasma has little effect on healthy cells."
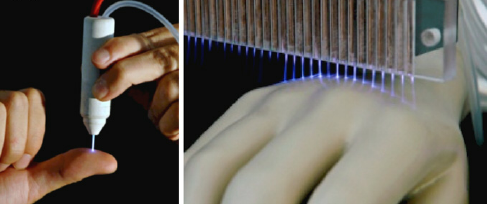
Images of cold plasma.
Old Dominion University researchers at the Frank Reidy Center for Bioelectrics have discovered a potential way to treat therapy-resistant cancer that exploits a common vulnerability in the malignant cells and minimizes some of the negative side effects for heathy tissues in patients.
Professors Michael Kong and Hai-Lan Chen led the study, which was done in conjunction with Huntsman Cancer Institute at the University of Utah.
The ability of cancer cells to adapt and develop resistance to current therapies accounts for approximately 90% of cancer-related deaths. The research by Kong and Chen showed that utilizing cold plasma, a specially engineered gas discharge composed of charged and highly reactive molecules, was very effective in killing cancer cells - without harming surrounding healthy cells. Importantly, this was achieved by reducing the intensity of the cold plasma well below the level commonly used to kill cancer cells with brute force.
"Because cold plasma contains many effectors that work as a team to rapidly kill resistant cancer cells at low intensity of cold plasma, the bystanders do not get killed," explained Kong, Batten Endowed Chair in Bioelectrics at ODU. "Instead of relying on the brutal force of a tiger, it leverages the teamwork of a lot of wolves."
The research was done on chronic myeloid leukemia (CML) cells from patients at the Huntsman Institute. Kong said CML is caused by a singular molecular event of mutation, giving it a clean-cut pathology.
"Because of this clean-cut pathology, efficacy data with chronic myeloid leukemia cells allowed us to establish a clear picture of the underlying mechanisms with little risk of ambiguity," said Chen, associate research professor in molecular biology.
Clinically, however, this pathology quickly leads to a rapid rise of resistance of CML to the treatment of targeted therapy.
"If you think about it, it's not surprising," Kong said. "If there is a single target, the cancer cells say, 'Well, I only have one area that I need to further mutate and evade that treatment.'"
The ODU researchers took advantage of cold plasma's diverse effectors to employ a siege strategy that exploited cancer cell's "supply lines" - oxygen, nutrients, and energy. This is a distinct vulnerability of cancer cells because of their need to aggressively grow the tumor.
"Our cold plasma system basically suppressed the supply lines to cancer cells to result in their death. Importantly, the cold plasma has little effect on healthy cells," Kong said. "In other words, our cold plasma enables a selective siege."
The tests involved applying the same dose to leukemia cells and blood samples from healthy individuals. In both cases, healthy cells did not die. They also applied cold plasma and cold plasma-activated liquid solution to mice and found the same result.
The reason for this, Kong said, is because the solution is not in one's system for long - up to 20 minutes. "They go there, they find the job, they're gone," he said.
In chemotherapy, by contrast, retention time is much longer, thus adding to toxicity by indiscriminately damaging cancer and healthy cells, he said.
"This is a highly promising and novel approach to drug resistance," said Dr. Brian Druker, director of the Oregon Health & Science University Knight Cancer Institute. Druker was not involved in the study but is widely recognized for his work in the development of targeted therapy for treatment of chronic myeloid leukemia.
Kong said the next step is take this to a clinical trial. He believes the "selective siege" treatment could work on other cancers, particularly those that are drug resistant or are being treated with targeted therapy, "because our approach really exploits the weakness of cancer cells in aerobic life."
"We should not be limiting ourselves," he added. "I want to see this happen in the real world. That would give me the ultimate satisfaction."
Kong and his team are also working on a cold plasma-activated gel treatment for vitiligo, an autoimmune disorder that causes the loss of skin color in patches and afflicts approximately 70 million people worldwide according to the Global Vitiligo Foundation.
The team formulated the plasma solution into a topical gel. A phase 2 randomized controlled clinical trial showed promising results - 80% of the participants had partial re-pigmentation, while the other 20% had 100% re-pigmentation. The next step would be a multi-centered phase-3 clinic trial, Kong said.
"What I'm really proud of is, coming from an engineering background initially with limited knowledge in biology and medicine, we went from the concept to engineering development technology to improve the delivery and really found some unique therapy and proved it in animal studies and clinical trials," Kong said.
Related News Stories
ODU Ranked No. 1 in Maritime Research Among U.S. Universities in Peer-Reviewed Study
The survey looked at the impact and volume of maritime publications by researchers over a 20-year period. (More)
ODU to Add Doctor of Occupational Therapy Degree
The full-time, 105-credit program in the College of Health Sciences would add a cohort of 40 to 45 students annually. (More)
ODU Biology Professor Part of Team Awarded $7 Million to Assess Climate Change Impacts on Coral Reefs
Daniel Barshis will be returning to American Samoa to conduct research from late January to early March. (More)